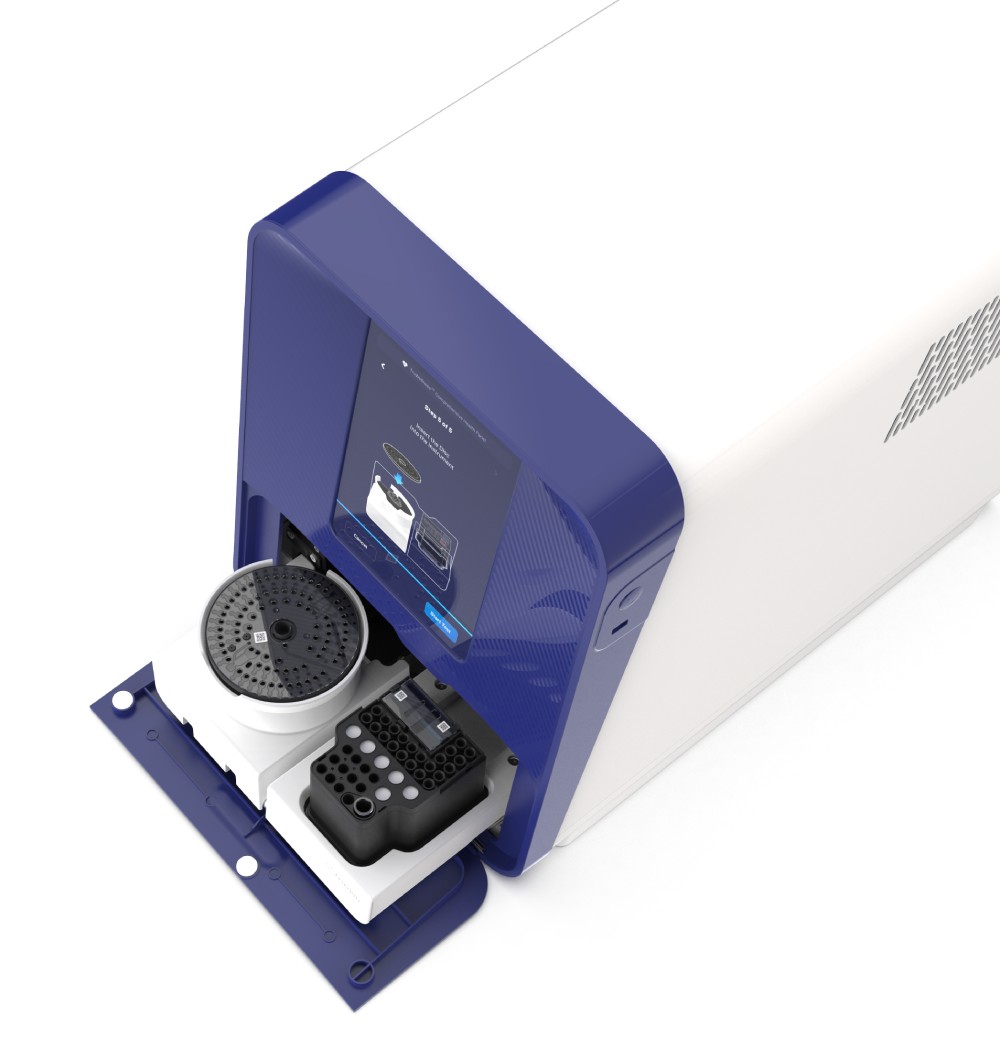
Reimagining Blood Testing
A few drops of blood. No send outs. Fully automated. Accurate results in minutes. Truvian is disrupting the blood diagnostics industry by developing an easy-to-use, automated benchtop blood testing analyzer. We’re elevating the standards and reimagining blood testing for convenience, simplicity and real-time results. Our technology is designed to provide lab-accurate results for a comprehensive suite of routine blood tests — all in a single run. Patients can receive immediate results during their appointment with their healthcare provider, enabling them to discuss those results and turn insight into action on the spot.